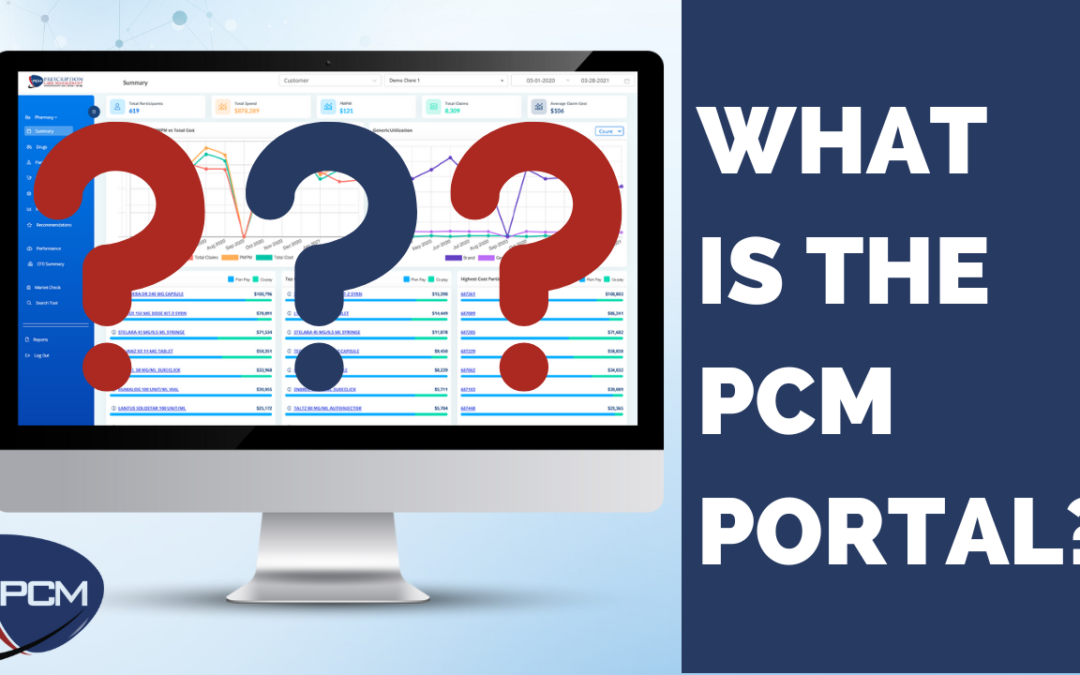
by Team PCM | Mar 10, 2023 | video gallery, Analytics, Broker, Platform, Recomendations, RFP Tools
What is the PCM Portal? Start simplifying by building an effective pharmacy program that fits your needs. Watch More Call 1-800-281-7050Fax 1-855-296-3933Email sales@pcmsavings.com Solutions Interactive Platform Data Integration & Monitoring Rx Benefit Plan...
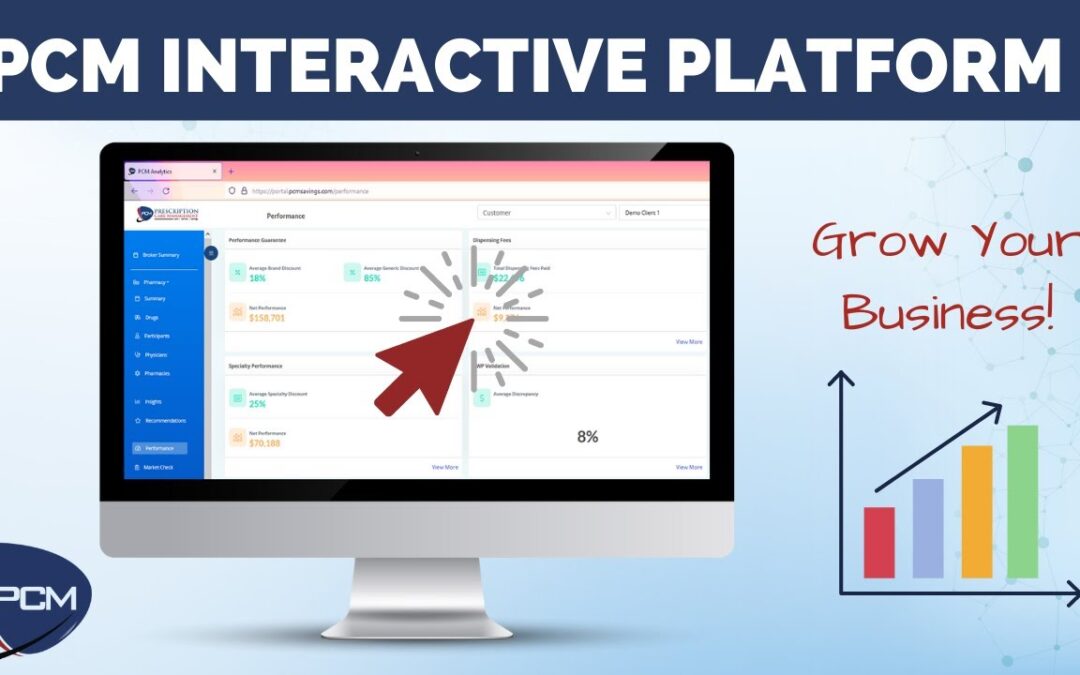
by Team PCM | Feb 3, 2023 | video gallery, Analytics, Broker, Platform, Recomendations, RFP Tools
Interactive Sales Platform Simplify sales and benefits management with a platform that optimizes your client’s benefit plan while providing claim-level data to validate benefit decisions. Watch More Call 1-800-281-7050Fax 1-855-296-3933Email sales@pcmsavings.com...

by Team PCM | Feb 3, 2023 | video gallery, Analytics, Platform, Recomendations
Visibility, Aggregation & Cost Containment Better reporting means more value for clients, less administrative work for you, and a stronger book of business. Let PCM help. Watch More Call 1-800-281-7050Fax 1-855-296-3933Email sales@pcmsavings.com Solutions...
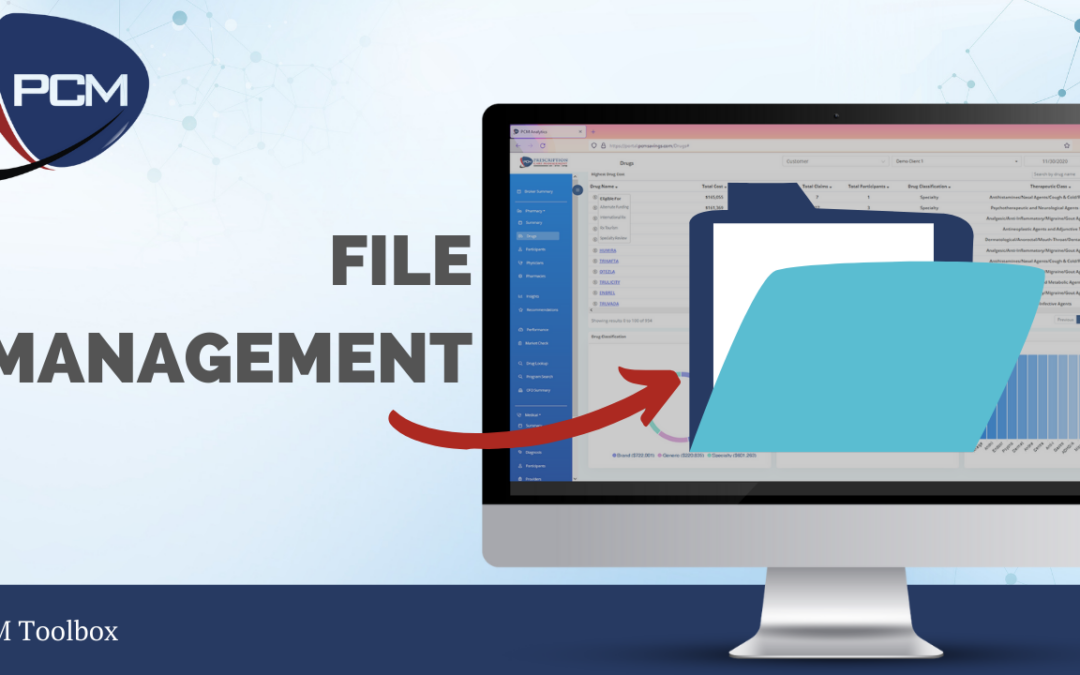
by Team PCM | Jan 26, 2023 | video gallery, Analytics, Broker, RFP Tools
PCM File Management Simplify file management, streamline your process, and spend more time growing your business with PCM Data Warehouse and PCM File Move. Watch More Call 1-800-281-7050Fax 1-855-296-3933Email sales@pcmsavings.com Solutions Interactive Platform Data...
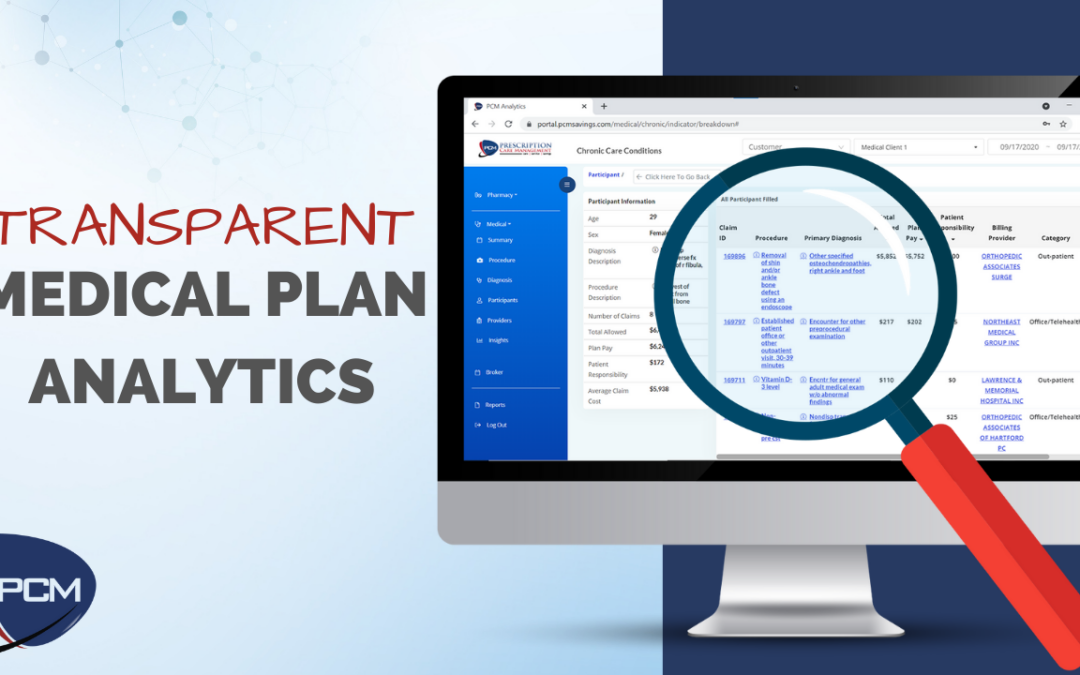
by Team PCM | Jan 26, 2023 | video gallery, Analytics, Platform
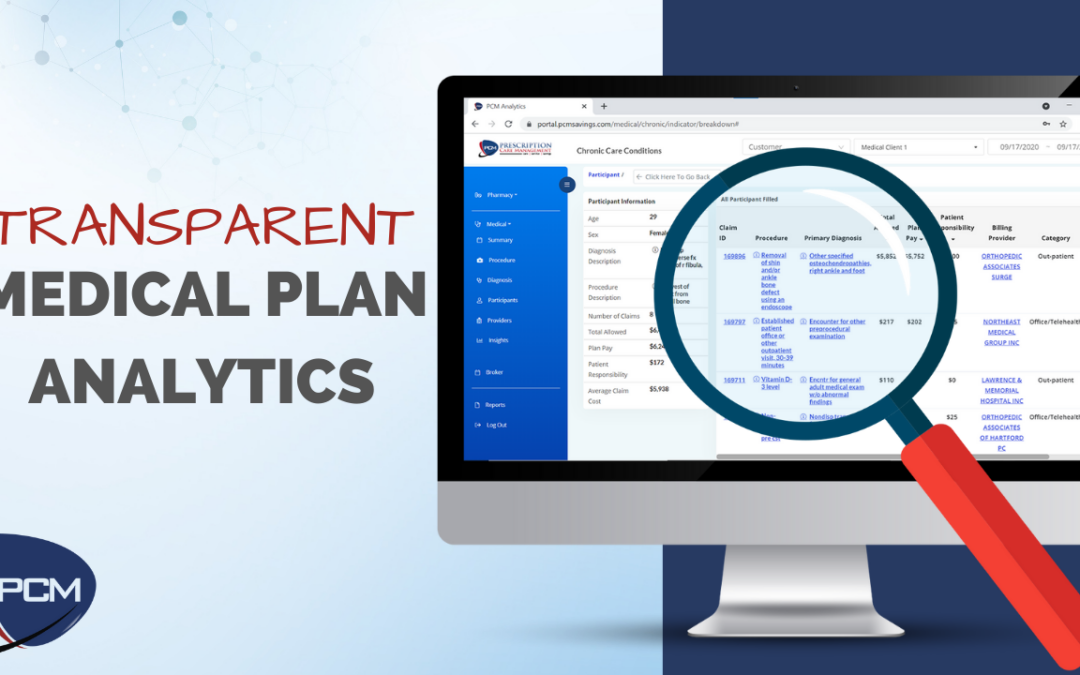
PCM Medical Analytics With PCM Medical Analytics, visibility, insights, and tools are just a click away. Watch More Call 1-800-281-7050Fax 1-855-296-3933Email sales@pcmsavings.com Solutions Interactive Platform Data Integration & Monitoring Rx Benefit Plan...

by Team PCM | Jan 26, 2023 | video gallery, Analytics, RFP Tools
PCM Rebate Management PCM provides the detail you need to own your rebates. Watch More Call 1-800-281-7050Fax 1-855-296-3933Email sales@pcmsavings.com Solutions Interactive Platform Data Integration & Monitoring Rx Benefit Plan Services Clinical Engagement Report...