Optimize Rx contract performance.
Complete dynamic contract performance audits and benchmark market PBM rates n half the time and at significantly less cost.

Why audit with PCM?
Plan audits, RFPs, and annual reviews eat up time and resources. With PCM’s Rx benefit plan services you can automate contract evaluation, validation, and monitoring.
Support Solutions
- Rx Market Check
- Rx Performance
- Rebate Management
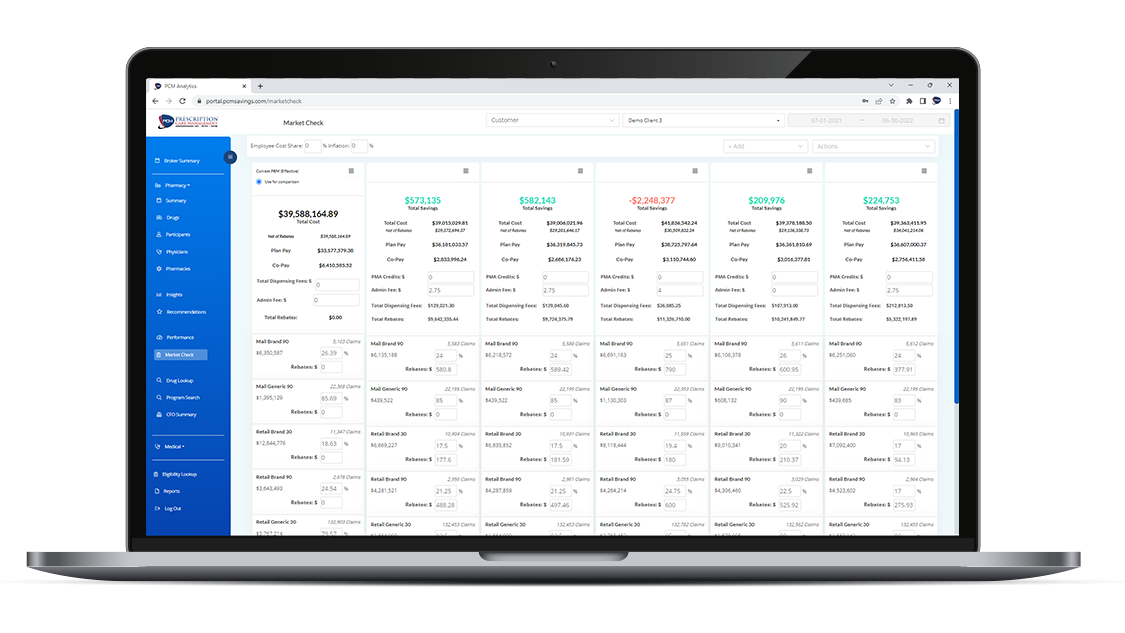
Rx Market Check
Driven by PCM’s interactive platform, Rx Market Check simplifies claims repricing and PBM contract comparison, dynamically benchmarking:
- Cost share
- Credits and fees
- Rebates
- Discounts
- Exclusions
- Trend
- Guarantees
Evaluate Multiple PBMs With a Click
Rx Market Check provides visibility and the ability to dynamically change key contract metrics for invaluable insight into pre-built or custom contracts.

Custom Contracts
Build custom contracts to find the best fit for each client. Evaluate the impact of unique contract guarantees, cost share, trend, and other metrics.

Standard Contracts
Utilize our 18 pre-built contracts from industry-leading vendors. Contract data is carefully vetted and updated to reflect current rates.
The Rx Market Check Process
PCM does the work. Our automated system and pharmacy experts allow you to easily compare validated contract rates without dedicating unnecessary time and resources to administrative work.
01
Automated Analysis
We load your data directly into our analytics system. And automated analysis aggregates and standardizes your data so your market check compares apples-to-apples.
02
Dynamic Comparison
Using our interactive platform, you can compare current PBM rates to other market contracts. Our system allows you to dynamically adust fees, credits, effective discounts, rebates, and trend to see available savings with different contract structures.
03
Report Generation
Use our native report builder to download market check findings within minutes, including line-by-line and claim-by-claim detail and a PDF summary report. Standard and custom reports are available with a click.
04
Expert Review
Review the market check findings with our pharmacy experts to ensure you find the contract that best fits the plan’s needs.
Data Transparency
As an independent third-party, PCM is committed to data visibility. Unlike other contract analysis vendors, we are not affiliated with any PBM or consultant and provide our partners with transparent, validated information, no strings attached.
For questions about the data we use and how to integrate your data into our automated systems, contact us today.
Contract Comparison for Support Your Strategies

Benefit Brokers
Easily compare multiple market contracts to simplify renewal and RFP management.

Plan Sponsor
Ensure your contract aligns with market rates with a validated comparison.

TPAs
Partner with brokers and consultants to simplify evaluation of self-funded contracts.

Consultants
Get a transparent look at plan, vendor, and contract data to better advise your clients.
Why PCM?
Use Case
Prescription Cost Management Best Practices: PBM Contract Market Check
Benefit consultants face significant challenges when managing pharmacy benefit spedn for clients. the lengthy process of evaluations PBM contracts for large employers often elaves limited time and resources for mid-market groups, resulting insuboptimal contract assessments due to resource constraints and complex PCM repricing.
This use case explores how one consultant utilized PCM technology to drastically reduce the time required for contract evaluation for a mid-market group from several weeks to a few busines hours.

See how PCM simplifies Rx benefit management.
See how PCM simplifies Rx benefit management.
Rx Performance
Ensure contracted agreements are being met with an automated Rx Performance review, validating:
- Guaranteed dispensing fees
- Rebates
- AWP discounts
- Specialty drug categorization
- Co-Pay tiers
Simplifying Rx Financial Audits
PCM’s Rx Performance tool compares actual claims data with PBM contract information to identify anomalies, errors, and unmet guarantees. Top to bottom analysis of the Rx Contract ensure the plan is receiving the best possible rates.

Review Contract Guarantees
Compare contract guarantees to plan received discounts to negotiate better rates.

AWP Mismatch
Evaluate mismatches between the provided and actual AWP to identify cost savings.

Rebate & Drug Exclusions
Pinpoint how overall plan spend is impacted by pricing and rebate exclusions.

Dipensing Fees
Identify claim level actual and contracted dispensing fee to ensure guarantees are met.

Drug Rebates
Prioritize drug rebates that positively impact plan spend with claim-level rebate review.

Specialty Review
Confirm specialty drug categorization and impact on by utilization.
Contract Performance With a Click
Utilizing PCM’s automated system and proprietary algorithms, benefit experts are shortening audit times from weeks to hours.
01
Automated Analysis
We load plan data directly into our analytics system. An automated analysis aggregates and standardizes the numbers to validate the RX contract performance.
02
Dynamic Analytics
Key performance metrics are displayed in our interactive platform, giving you a claim-level view of your contract, validating contract guarantees. Native reports include claim level detail and summary charts for easy evaluation.
03
Expert Service
Our expert team evaluates performance results with you, ensuring data integrity and transparency. We provide plan recommendations based on years of audit experience so you can have complete information to make faster plan decisions.
Complete data transparency to drive global plan decisions.
Rebate Management
As advertised, drug rebates should provide savings on high-cost drugs, but they may be driving up costs, resulting in an inflexible formulary, opaque net-cost metrics, inaccessible pricing details, and limited cost-containment integrations.
PCM supports benefit experts in identifying and implementing a low net-cost rebate management strategy.
Create Client-Specific Formularies
PCM supports you in building a formulary based on lowest net-cost, not misaligned incentives.

Comprehensive Reporting
Use our robust reporting tool to identify drug-level trends and employ lower net-cost strategies, including insights into savings programs, pricing, and exclusions.
Plan Flexibility
PCM’s proprietary program supports you in controlling formulary changes, managing prior-auth protocols, and improving clinical outcomes.
Optimize Rebates
Analyze your existing claims data to identify plan rebates and
highlight true net-cost at the drug level.
- Easy cost-containment integrations
- In-depth drug level reporting
- Improved clinical outcomes
Improve plan efficiency and optimize rebates with PCM.
Optimize
Rx contract
performance.
Complete dynamic contract performance audits and benchmark market PBM rates in half the time and at significantly less cost.

Why audit with PCM?
Plan audits, RFPs, and annual reviews eat up time and resources. With PCM’s Plan Insight and Management tools you can automate contract evaluation, validation, and monitoring.
Support Solutions
- Rx Market Check
- Rx Performance
- Rebate Management
Rx Market Check
Driven by PCM’s interactive platform, Rx Market Check simplifies claims repricing and PBM contract comparison by dynamically benchmarking:
- Cost share
- Credits and fees
- Rebates
- Discounts
- Exclusions
- Trend
- Guarantees
Evaluate Multiple PBMs With a Click

Standard Contracts
Utilize our 20+ pre-built contracts from industry-leading vendors. Contract data is carefully vetted and updated to reflect current rates.

Custom Contracts
Build custom contracts to find the best fit for each client. Evaluate the impact of unique contract guarantees, cost share, trend, and other metrics.
WHY PCM
PCM does the work.
Our automated system and pharmacy experts allow you to easily compare validated contract rates without dedicating unnecessary time and resources to administration work.
- Independent
- Flexible
- Agnostic
- Responsive
Rx Performance
PCM’s Rx Performance simplifies financial audits by comparing actual claims data with PBM contract information to identify anomalies, errors, and unmet guarantees.
Top to bottom analysis of the Rx Contract ensure the plan is receiving the best possible rates.
WHY PCM
The Performance process is simple.
We load plan data directly into our analytics system, aggregating data to validate numbers. Built-in reporting provides claim-level and summary view of performance results. Our expert team walks with you through the analysis, arming you with complete plan information for faster decision making.
- Automated analysis
- Data visibility
- Expert service
Rebate Management
Create client-centric formularies.
PCM supports you in building a formulary based on lowest net-cost, not misaligned incentives. Analyze your existing claims data to identify plan rebates that benefit the plan and participants, not a third-party vendor.
Plan Flexibility
PCM’s proprietary program supports you in controlling formulary changes, managing prior-auth protocols, and improving clinical outcomes.

Comprehensive Reporting
Use our robust reporting tool to identify drug-level trends and employ lower net-cost strategies, including insights into savings programs, pricing, and exclusions.
WHY PCM
Optimized Rx Rebates
PCM simplifies rebate management, balancing clinical efficiency with cost containment.
- Plan carves out rebates from PBM contract.
- PCM assists plan in submitting rebates to aggregator.
- Rebates, combined with drug-level reporting, provided to plan.

CONTACT
SOLUTIONS
COMPANY
LEARN MORE
© 2024 by Prescription Care Management
See how PCM supports you.
Ready to learn more?
PCM provides the visibility, insights, and tools you need. Want proof? Click here to schedule a demo.

Call 1-800-281-7050
Fax 1-855-296-3933
Email sales@pcmsavings.com
Solutions
Interactive Platform
Data Integration & Monitoring
Rx Benefit Plan Services
Clinical Engagement
Report Builder
Company
Contact
About
Privacy Policy
Terms of Use
Press Releases
PCM Premier Formulary
Learn More
Blog
Archive
Security Certifications
Upload

© 2024 by Prescription Care Management
